Hunting the mysterious source of a global illness
As Kawasaki disease is on the move, hitting kids across the planet, researchers team up to identify its cause

The view from a plane in which atmospheric scientists are taking air measurements over Japan. They’re looking for airborne particles that might prove a trigger for Kawasaki disease.
Roger Curcoll, IC3
Shortly after World War II, a mysterious disease started showing up in Japan, mostly in young children. Now known as Kawasaki disease, it’s named for the doctor who first reported it in his young patients. Symptoms include bloodshot eyes, a swollen tongue and a high fever. Especially curious, the skin on a child’s hands will begin to peel.

Most victims of this disorder are under age 5 and tend to recover within a couple of weeks. But not all are so fortunate. Some may develop permanent, life-threatening heart problems.
By the 1970s and 1980s, the disease had started showing up in Hawaii and California. Today, Kawasaki is still spreading. Cases have emerged in 60 different countries and in all U.S. states. The illness has appeared on every continent. Yet it’s more common in some countries than others.
For instance, up to 1,667 out of every 100,000 Japanese children will get it. But out of 100,000 U.S. kids, fewer than two dozen will come down with the disease. Still, even U.S. cases are numerous. Every year, Kawasaki disease sends some 5,000 people to American hospitals. (For perspective, that’s more than twice the number sent to the hospital with food poisoning by the common germ, E. coli O157.)
Researchers have worked for decades to find what causes Kawasaki disease. So far, they’ve come up empty-handed. It’s become a puzzle that doctors and scientists all over the world are now trying to solve. If they knew what caused the illness, they might have a shot at preventing it.
The disease hits healthy kids suddenly, with no warning. Any child can fall sick. Still, it’s most common among kids of Asian or Pacific Island descent. Fortunately, the disease doesn’t travel from person to person, as many diseases do. That means sick kids can’t infect others.
“Kawasaki disease just doesn’t look like or act like any disease we’ve ever known. It’s something new,” says Jane Burns. She’s a pediatric infectious disease specialist. She works at Rady Children’s Hospital of San Diego in California. There, she specializes in treating young Kawasaki patients.
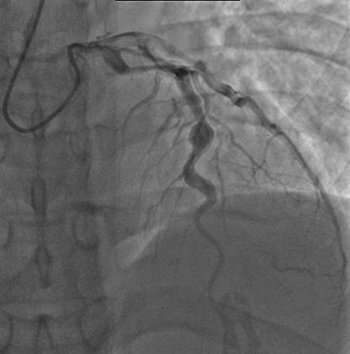
What drives her? Some children suffer devastating impacts. Roughly one in five of its victims, for instance, develop permanent heart damage. The walls of their arteries — the vessels that carry blood away from the heart to the rest of the body — become inflamed or swollen. Inflamed arteries can lead to blood clots, sticky masses of red blood cells. If clots block blood from flowing in the heart, they can trigger a heart attack.
Most doctors suspect that something in the air leads to Kawasaki disease. A trigger is a substance or event that sets off disease symptoms. Some Kawasaki researchers suspect the trigger for this disease is in the environment. So with help from scientists who study Earth’s weather and atmosphere, they’re screening for the possible agent. Other researchers believe a new virus may be at fault.
No matter who’s right, experts hope to discover the cause of Kawasaki disease with an eye to one day halting its spread.
Story continues below video.
An airborne discovery
Burns began working on Kawasaki disease in the 1980s. Early on, she noticed a pattern in her San Diego clinic. She seemed to see more patients with Kawasaki disease during the late winter and early spring. “March was always a really big month,” she says.
She began to collect weather data from the local airport. “It wasn’t very scientific,” she admits. But “when it rained, we seemed to see a bunch of new patients.”
Burns didn’t know what it meant or whether that was important. But it appeared climate was somehow linked to Kawasaki disease. And she wasn’t the only one to notice this.
Doctors in Japan reported a similar pattern. There were three major epidemics of Kawasaki disease in Japan in the 1970s and 1980s. An epidemic happens when many more people than expected get a certain disease in a short period of time. These epidemics happened in April 1979, May 1982 and March 1986. The Japanese doctors also found that Kawasaki disease seemed to cluster in certain parts of the country. Several regions had many cases while others had few.
Burns began to wonder whether something in the environment was the trigger.
Turning to computers for help
She had heard an ocean scientist give a talk about how changes in ocean temperatures in one part of the world could affect the climate in faraway areas. She asked that scientist whether seasonal patterns in Kawasaki disease in San Diego might be connected to outbreaks across the Pacific Ocean.
The researcher put Burns in touch with Xavier Rodó. The thought was that this atmospheric scientist might be able to help answer her question.
In fact, Rodó now notes, “Our atmospheric research introduced to this problem a new way of looking at Kawasaki disease.” Rodó works in Barcelona, Spain, at the Catalan Institute for Research and Advanced Studies. There, he uses physics and math to make computer models. For his Kawasaki research, he used the models to probe how changes in climate and weather in one place might influence disease patterns elsewhere around the world.
Rodó and Burns teamed up with doctors and scientists in Japan. The Kawasaki disease trigger appeared to be something children were inhaling. So they began to look for a trigger in the troposphere. That’s the layer of Earth’s atmosphere that extends from the ground to a height of about 10 kilometers (roughly 6 miles).
In winter, strong winds from Asia blow across the islands of Japan from the northwest. Rodó discovered that when winds blew from this direction, Kawasaki disease cases in Japan spiked. Those winds appeared to come from Central Asia. Disease cases dropped again when the winds shifted and now blew from some other direction.
Rodó also compared winter peaks of Kawasaki disease in California and Hawaii with when the disease peaked in Japan.

This turned up something striking. The same northwesterly wind patterns that predicted Kawasaki disease in Japan also predicted cases in the United States.
To Rodó, it appeared that the winds must be blowing the source of Kawasaki disease across the Pacific.
Air masses are large blobs of air with one temperature and humidity. They drive the weather. Wind currents act like huge conveyor belts. They can carry air masses thousands of miles. So if the wind is blowing from a certain direction, the same air mass that crosses over Japan can ride the conveyor belt, arriving in California five days later, explains Mark Thiemens. He studies air chemistry at the University of California, San Diego.
Rodó looked at air masses that had crossed over Japan during the three Kawasaki disease epidemics in the 1970s and 1980s. He compared them to air masses that crossed over Japan each year during California’s winter peaks of Kawasaki disease.
All seemed to come from the same place. It was a farming region in northeast China.
Homing in on the source
Burns suspects that a windborne toxin — some natural poison — comes from this area of China to trigger Kawasaki disease. Researchers now are scouring the region to find it.
Some evidence suggests a fungus might be the source. Rodó and Japanese scientists sampled air from a plane as it flew over Japan. Aerosols are microscopic particles — from pollen and water vapor to soot and pesticides — that can travel in air masses. (Fog, haze, dust and smoke are examples of aerosols.) The researchers collected aerosols from high up in the atmosphere and measured their quantities at a time in winter when cases of Kawasaki disease peak.
Rodó found high levels of Candida, a type of yeast, in the air blowing over Japan. More than 20 species of this one-celled fungus have been linked to diseases in people. Found across the globe, cells of this yeast show up on leaves, flowers, water and soil.

Peter Lillian, a high school student volunteering in Burns’ lab, found another clue. Peter had been fascinated by Kawasaki disease ever since his little brother contracted it. So in 2012, “I started talking with Dr. Burns about her research and ways I could get involved,” Peter recalls. (He’s now a college student at the University of Southern California in Los Angeles.)
Burns sent Peter to the library with an assignment: Learn about the history of the region in China where the trigger for Kawasaki disease seemed to come from. He spent a summer poring over translations of Chinese newspaper stories and farm records from after World War II. During that time, he learned, growers raised a lot of sunflowers in northeast China. They pressed the sunflower seeds to extract oil for cooking. Around the same time that Kawasaki cases started to emerge in Japan, the Chinese began to burn leftover husks, or shells, from sunflower seeds as fuel.
Fungi are found naturally on those husks. Peter wondered whether burning them might spew fungal cells into the air.
Researchers are now investigating Peter’s theory by going to the source. Thiemens, the air chemist, is setting up monitoring stations on the ground in northeast China. He’ll measure gases and collect air particles. He’s looking for patterns that could connect specific on-the-ground activities — like burning fuel — with Kawasaki disease cases in Japan and the United States.
Thiemens isn’t sure what he’ll find. “It’s a mystery, but that’s what makes science fun,” he says.
Viral possibilities?
Not all Kawasaki disease researchers agree with Burns’ fungal-toxin theory. Anne Rowley is a pediatric infectious disease specialist at Northwestern University in Chicago, Ill. She believes Kawasaki is a viral disease. “When you look at patterns of Kawasaki Disease — who gets it, when and where — pretty much everything about it is consistent with a viral infection,” she says.
Viruses are tiny infectious particles. They typically enter the body through the nose or mouth — when someone eats, drinks or breathes. “If we can find out what the virus is, then we can develop a vaccine to prevent it,” says Rowley.
Viruses spread in the body by making copies of themselves. They do this by hijacking a cell’s machinery. They insert their own DNA into a cell’s nucleus. This leaves behind clumps of virus particles, “almost like a footprint,” explains Rowley.
Pathologists found these viral footprints in the heart cells of children who had died from heart problems after Kawasaki disease. (Pathologists are doctors who study tissues, organs and bodily fluids to diagnose disease. They’re often the people who perform autopsies to learn what caused someone’s death.)
A footprint may be a clue, but it still doesn’t explain what causes Kawasaki disease. Rowley is hopeful they’ll find its source — and soon. “We’re inching closer, but the world of viruses is huge,” she says. “We know only a tiny fraction of them.”