Vaccines help everyone — even the unvaccinated
Here’s why falling vaccination rates worry doctors, cancer patients and parents of young babies

Most people think that vaccines only help those who get that shot in their arm. In fact, vaccines also limit the spread of disease to people who, for medical reasons, cannot be vaccinated.
monkeybusinessimages/iStock/Getty Images Plus
Kids’ cuts and scrapes are rarely a big deal. But one six-year-old boy in Oregon nearly died after getting a cut on his forehead while playing outside. Six days after the accident, his jaw began clenching. Muscle spasms wrenched his arms. His neck and back arched out of control. Then the boy had trouble breathing. Emergency medical personnel airlifted the child from the family farm to a hospital. Doctors quickly figured out the problem: tetanus.
The bacteria that cause tetanus are everywhere, notes the Centers for Disease Control and Prevention (CDC) in Atlanta, Ga. Luckily, there’s a vaccine that can prevent tetanus. But the boy’s parents wouldn’t let him get it.
As a result, the child became so sick he had to spend 57 days in a hospital. For more than a month of that time, he needed a breathing machine. After the hospital, he had to spend 17 more days in a health-recovery center. The treatment was costly: $811,929. And that didn’t cover the cost of airlifting him to the hospital when his symptoms turned deadly.
Eventually, the boy got better. Yet even after doctors explained the tiny risks and huge benefits of vaccines, his parents refused follow-up doses of vaccine for their son.
Doctors described his case in the March 8 issue of Morbidity and Mortality Weekly Report (MMWR).
“Vaccines are safe. Vaccines save lives,” says Peter Hotez. “They are the most effective public health technology ever invented.” He’s a pediatrician and vaccine scientist at Baylor College of Medicine and Texas Children’s Hospital. Both are in Houston.
Most people gladly get vaccines for themselves and their children. Yet a small share of people says no. In fact, the percent that turns them down has been climbing. That is putting more children at risk. And it endangers the health of others, from babies to cancer patients and more.
“We’ve reached a point where so many children are not being vaccinated, that we’re seeing a return of dangerous and even deadly infectious disease,” Hotez says.
Protection from disease
Vaccines work by arming the immune system to fight off a disease. “A vaccine gives your body a little sample of what a virus or bacterium looks like,” explains Danielle Koenig. She’s a health educator with the Washington Department of Health in Olympia. A vaccine prompts the immune system to make germ-killing antibodies. Later, if you’re exposed to those germs, “your body has those antibodies ready to go.”
But that’s not all. Many vaccines help protect other people from infections. As more and more people get a vaccine, the disease has fewer people it can infect. And that’s the first step in slowing or even stopping its spread. Public health experts call this herd immunity.
Herd immunity works like a shield or force field to protect those people who are most at risk because they cannot be vaccinated, Koenig says. “The more people who get vaccinated, the stronger that field is.” On the flip side, “if not enough people are immunized, that force field breaks down and there are holes in it.”
Herd Immunity:
Measles is a disease that causes high fevers, coughing, a sore throat and an ugly rash. One or two in every 1,000 people who get measles will die from it, the CDC notes. Many more will end up with pneumonia, brain infections and nervous-system damage, such as deafness. Measles also makes it hard to fight off certain other diseases for the next two to three years.
“Measles is a very dangerous disease,” observes Jonathan McCullers. He is a pediatrician at the University of Tennessee Health Science Center and Le Bonheur Children’s Medical Center in Memphis. He’s also a faculty member at St. Jude’s Children’s Research Hospital in the same city.
In contrast, “the vaccine against measles is very safe and very effective. One dose provides protection in about 93 percent of individuals,” McCullers says. A second, booster dose bumps the protection up to 97 percent. And, he notes, “Very few side effects occur.”
Herd immunity also protects individuals who can’t be vaccinated. This includes babies who are too young to get vaccines. It also counts cancer patients and others with weak immune systems. About one in eight U.S. children and teens depend on herd immunity to protect them from measles. This also includes about 3 in every 100 people for whom a vaccine might not offer full protection. And it counts children whose parents say no to vaccines. These people can still become infected. But they’re far less likely to get sick because of herd immunity.

Measles is only one of many diseases for which there is a vaccine. Another is pertussis (Pur-TUSS-is), which triggers a severe hacking cough. (In babies it is known as whooping cough, for the sound of their coughs.) This infection can cause pneumonia, convulsions, brain disease and breathing problems.
A tetanus vaccine could have prevented the disease that almost killed the Oregon boy. Other diseases that a vaccine could prevent: diphtheria (Dip-THEER-ee-uh), which makes it hard to breathe and can lead to heart failure. There’s also rotavirus, which causes severe and sometimes deadly diarrhea. Vaccinations can prevent chickenpox, which produces fever, a rash and sometimes serious nerve damage in later life (known as shingles). Vaccinations can also prevent Rubella (Rue-BEL-lah), which can trigger fetal deaths in pregnant women.
And then there’s the yearly vaccine against flu. This common infection kills tens of thousands of people in the United States each year. Teens also need vaccines for human papillomavirus (Paa-pil-LOH-muh-vy-rus) and meningococcal (Meh-NIN-jo-KOK-ul) disease. The first of these can lead to cancer. The second attacks the nervous system and blood stream.
Diseases most people don’t have to get, now, thanks to vaccines:
-
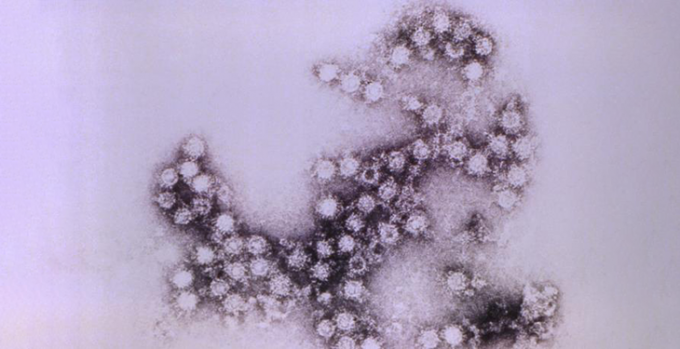
The Coxsackie B4 virus particles, shown here, could cause life-long debilitating muscle damage that left some its victims paralyzed. Once polio vaccines became available, this highly infectious disease all but disappeared. CDC -

The potentially life-threatening tetanus — also known as lockjaw — is caused by infection with Clostridium tetani bacteria (stained here in with methylene blue). CDC -
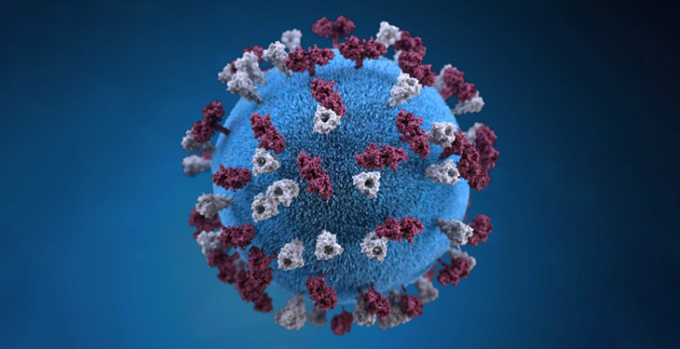
This illustration shows what a measles virus looks like. Just since the year 2000, vaccinations have saved more than 20 million people from dying of this disease. Allison M. Maiuri/CDC -

These Corynebacterium diphtheriae bacteria are responsible for causing diphtheria, a disease that can obstruct the airways, sometimes killing its victims by suffocation. CDC -
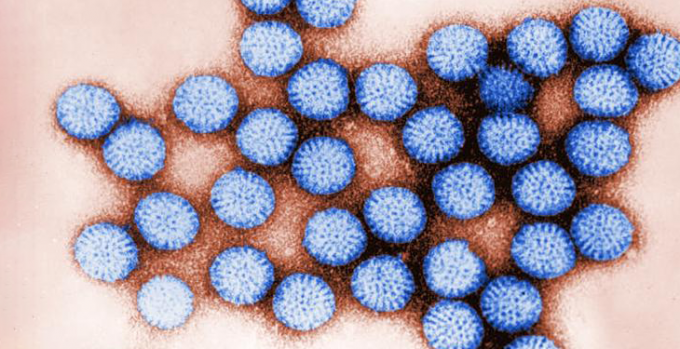
Rotavirus, stained blue in this electron micrograph, occurs most commonly in young children. It causes fever, tummy aches and watery diarrhea. Some children die from the disease. Vaccines can’t always prevent the sickness, but they can greatly limit its severity. CDC -
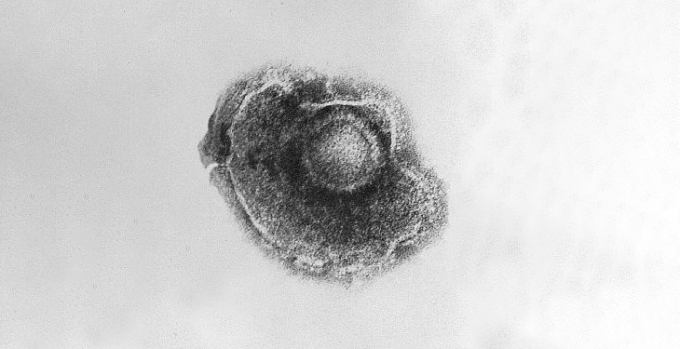
This Varicella zoster virus is responsible for chickenpox, a highly contagious disease. It can cause a fever, an itchy blistering rash and exhaustion. Cynthia Goldsmith/CDC -
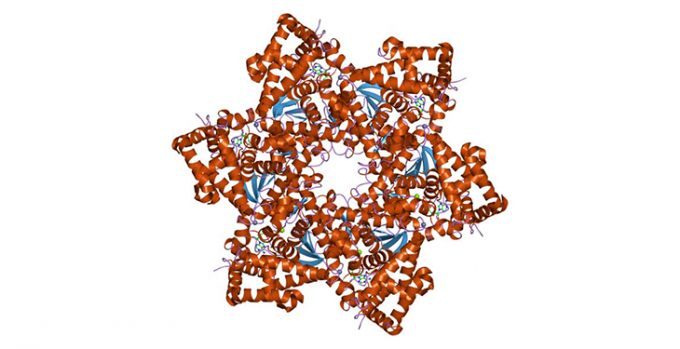
There are some 150 different human papillomaviruses (like the one illustrated here). They currently infect about one in every four Americans. The most common sexually transmitted disease, it can cause warts or no symptoms at all. But infected people are at a heightened risk for later developing cancer in the genitals. Jawahar Swaminathan, MSD staff/European Bioinformatics Institute/Wikimedia Commons [Public domain] -

The Neisseria meningitidis bacterium (in blue) causes meningococcal disease. Symptoms include fever, headache and a stiff neck. It can also cause severe disease if it infects the brain, spinal cord or bloodstream. Once symptoms occur, the disease can turn deadly in hours. Kids, teens and young adults are most at risk. Charles-Orszag et al./Nature Communications, 2018/Wikimedia Commons
A growing problem
On March 5, 18-year-old Ethan Lindenberger of Norwalk, Ohio, spoke to lawmakers in Washington, D.C. The high school student spoke of how his mother wouldn’t let him get vaccines when he was little. As a teen, he learned about the science behind vaccines. He talked with his mom, but she still said no. When he turned 18, Ohio law said he no longer needed his parents’ okay. So Ethan finally got those vaccines. But for 18 years he was at risk.
Lindenberger didn’t get measles as a child. He also didn’t get other infections that vaccines could prevent. And he credits herd immunity for that. “The people around me were vaccinated,” he tells Science News for Students. “Other people’s concern for safety was keeping me safe.”
In turn, Ethan felt concern for others. So when he was legally able to, he got vaccinated. “I saw that getting vaccines not only protects yourself but other people, and that was a big thing for me,” he says.
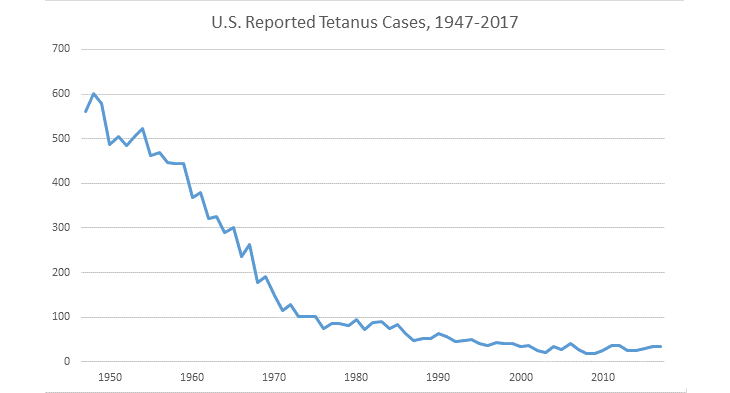
Before a measles vaccine became available in 1963, there were nearly half a million U.S. cases each year, of which nearly 500 died, the CDC says. Thanks to vaccines, though, the United States eliminated measles in 2000. And since 2000, the vaccine has prevented more than 21 million deaths worldwide, according to a November 30, 2018 report in MMWR.
However, unvaccinated travelers can still bring the airborne virus into the country from places where the disease is common. Already in 2019, New York, Texas, Illinois, Michigan, Oregon and Washington have been fighting outbreaks. As of March, most patients in the Washington outbreak had never been vaccinated for measles.
Since 2011, CDC reports there have been more than 2,100 cases of measles — 268 so far this year. Outbreaks happen elsewhere, too. Europe had more than 82,000 cases in 2018. Brazil had more than 10,000 cases that year. Those data come from the World Health Organization and the Pan American Health Organization.

Vaccine-preventable diseases should be on the decline. However, that is no longer true for some of these diseases. That’s because not everyone who can be vaccinated gets their recommended vaccines. As of 2017, about 13 in every 1,000 children under age two had never gotten a vaccine. That’s more than four times as many as in 2001, the CDC reported last year.
That 13 in every 1,000 may sound like a tiny number. But 3.86 million babies were born in the United States in 2017. So if the rate stays the same, that’s more than 50,000 more unvaccinated kids each year.
All U.S. states have laws that say children must get certain vaccines to attend school or daycare. A small share of those kids can’t get vaccines for medical reasons. And the laws allow for that. But the vast majority who don’t get vaccines have no medical exemption. As of 2018, 47 states allowed parents to say no for religious reasons. And laws in 18 states now let parents say no based on just their personal beliefs.
Saad Omer is an epidemiologist — a disease detective — at Emory University’s Vaccine Center in Atlanta, Ga. For a 2016 study, he led a team that reviewed 18 reports on measles outbreaks. More than half the people who were infected had never gotten the measles vaccine. And seven in every 10 of these people had no medical reason. That shows that vaccine refusals play a role in causing and spreading measles, the team concluded. Omer talked about his team’s findings at the same hearing where Ethan spoke.
Herds at risk
Herd immunity only works if enough people in a group have had their vaccines. The exact number depends on how fast a disease spreads and other factors. Measles is very contagious and spreads through the air. On average, Hotez explains, for every one person who gets measles, 12 to 18 more will now get it, too — “if they’re not vaccinated.” Measles outbreaks show up first when people skip vaccines, he says.

So public health officials aim for a 92 to 95 percent vaccination rate.
Some places are near or already below that threshold. In 2018, the rate for measles vaccination in Arkansas was just under 92 percent. This and other states also have “pockets” where clusters of vaccine-refusers live, says McCullers.
Even if a state’s overall rate is high, those clusters may be below the levels needed for local herd protection. Outbreaks can then spread easily there. And from there, they can “spill out into other populations,” McCullers says. That poses a big problem for children and other people who have no protection.
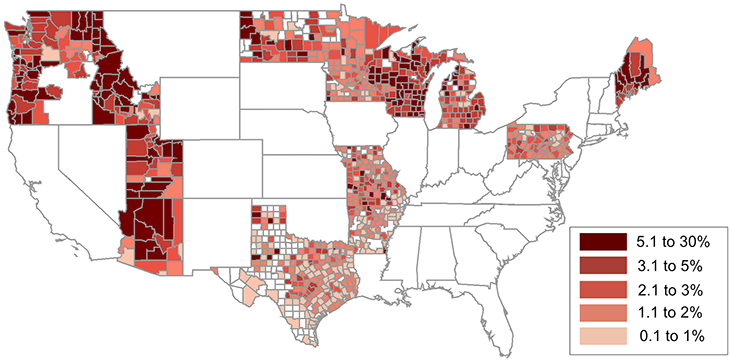
Arkansas isn’t the only place with areas like that. In a 2018 study, Hotez and others identified U.S. “hot spot” counties, ones with the most nonmedical refusals. Parents of more than one in every 20 children in those places had said no to their getting vaccines.
“We found more than 100 hot spots like that in the country,” Hotez says. Rural Camas County, Idaho, had the highest rate (nearly 27 percent unvaccinated) — or more than one in every four kids. The list also has several urban counties with recent measles outbreaks. They include counties around or near Portland, Ore., Detroit, Mich., and the Texas metro areas of Houston, Fort Worth and Plano. His team identified those hot spots last June in PLOS Medicine.
It doesn’t take a big drop to cause problems, either. Hotez and a colleague found that just a 5 percent drop in vaccination rates could triple the number of measles cases each year for U.S. children aged two to 11. And the public health costs of dealing with those cases would be an extra $2.1 million per year. Hotez and Nathan Lo reported those findings in the September 2017 JAMA Pediatrics.
What can be done?
In a sense, vaccines are victims of their own success, Ethan notes.
McCullers agrees. “If they work really well, nobody sees the disease for 30 years, and you get really complacent,” he says. But when a disease reemerges, people see the awful impacts. The little boy in Oregon was just “a regular kid who scrapes his forehead,” McCullers says. “Then he’s in the hospital for months with this horrible and painful disease.”
More education for parents may help avoid such problems. Starting in 2011, Washington state law has made parents get counseling from a licensed healthcare provider before they can refuse vaccines for their children. Vaccination rates went up for all but one available vaccine once the law was in effect. Omer and others reported that news last year in Pediatrics.
Policy makers can take action, too. As of March 2019, Oregon lawmakers are considering a bill to end non-medical exemptions from required vaccines. Another idea might be for lawmakers to lower the age when teens can get vaccines on their own. In most states that’s now age 18. However, some states let “mature minors” give their own consent.
What if you need your parents’ permission to get vaccines? Talk with your pediatrician or family doctor, Hotez suggests. Ask about your options. Your doctor may help talk to your parents as well.
“Be respectful, and be as kind as you can be,” when you talk with a parent or guardian, Ethan advises kids and teens. Although he says his mom was wrong about vaccines, he knows she loves him. So he keeps sharing the facts with her. He hopes his four younger siblings will eventually decide to get their vaccines.
Most people who reject vaccines “are coming from a fear-based, emotional place,” says Koenig at the Washington State Department of Health. “We suggest appealing to their brain and their heart. Understand where they’re coming from, and acknowledge that they want the best for their family.” Then try to address those feelings, she says, while staying true to the science.
If someone worries about side effects, for instance, focus on what any real side effects are — instead of ones spread through misinformation. Then you can talk about the much greater dangers of getting a preventable disease. Or, if someone thinks vaccines are gross, talk about how disgusting disease impacts can be. Those suggestions come from Matthew Motta. He’s a political scientist at the University of Pennsylvania in Philadelphia. He studies science communication and public policy impacts when people reject science.
Promote sound science about vaccines on social media too, suggests McCullers. Just as teens used social media to spread the word about school strikes for climate action, young people can speak out about the importance of vaccines, he says. “Now one teen has one voice, and that voice can go around the world.” (And yes, you can link to this article!)
Share personal stories and concerns as well, McCullers says. Think about the people you care about, and speak up for them. Maybe you have a baby brother, sister or cousin who could be in danger from unvaccinated people. Perhaps you don’t want your grandparents to face more risks from flu or other illnesses. You might also have a friend or family member whose immune system is weak because of cancer or another disease.
Full disclosure: My daughter Bethany died from cancer in 2018. Treatments weakened her immune system. So an infectious disease could have made her sicker or killed her. I echo what her husband Jarrod wrote on Facebook: “I got an extra two-and-a-half years with Bethany because everyone who loved her listened to our requests and was vaccinated against diseases that are easily dealt with.”